Home <Services < Cardiology < Atrial Fibrillation
Atrial Fibrillation treatment in Sinhagad Road Pune
What is atrial fibrillation?
Atrial fibrillation (AF or Afib) is a heart rhythm disorder. It can come and go of its own accord or be persistently present.
It is characterised by 3 features:
- The heart beats irregularly
- The heart beats less effectively
- The heart rate can be excessively fast or excessively slow
The science:
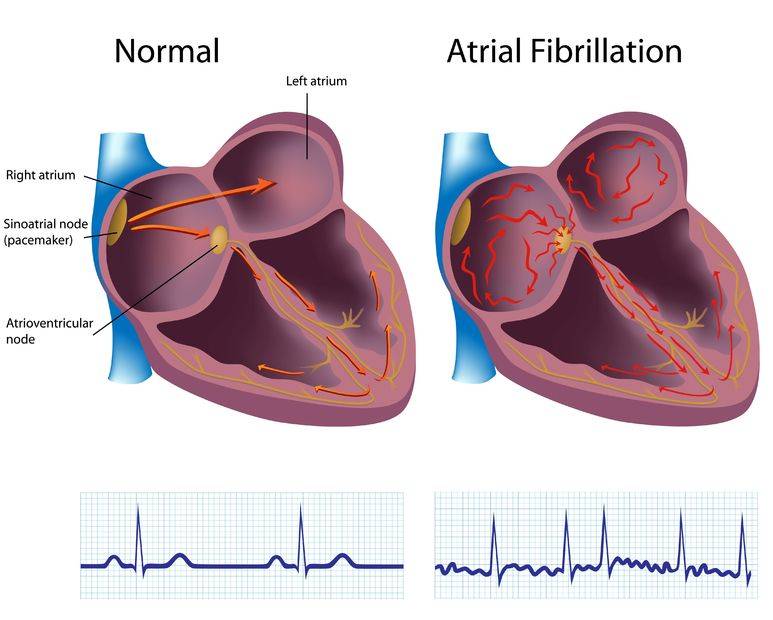
A normal heart has 4 chambers – two atria and two ventricles. The ventricles are the main pumping chambers and are responsible for pumping blood around the body and to the lungs. To pump blood out effectively, the ventricles need to fill with as much blood as possible. Whilst the majority of ventricular filling happens passively due to a suction effect, the atria sit at the top of the ventricles and help push some blood actively (also called the atrial ‘kick’) into the ventricles thereby increasing the effectiveness of each ventricular contraction.
Contraction of the heart is controlled by an electrical system and this is regulated by the sino-atrial node (otherwise known as our natural ‘pacemaker’). The sino-atrial node is located at the top of the right atrium. In atrial fibrillation the ability to conduct electricity through the atria is altered and electrical activity in the atria can become chaotic and irregularly irregular and therefore atrial fibrillation is always characterised by an irregularly irregular heart rhythm. The sion-atrial node is responsible for ensuring that our heart beats don’t go excessively fast or excessively slow unnecessarily. However in atrial fibrillation, the sino-atrial node is not able to regulate the heart rate as well and therefore the heart rate can go excessively fast or excessively slow and out of keeping with the body’s necessary requirements
In atrial fibrillation, the atria stop contracting and therefore the ventricles don’t fill with as much blood and as a consequence, less blood is pumped out with each ventricular contraction. It is thought that in a normal heart, the atria contribute to about 15-20% of ventricular filling and therefore in atrial fibrillation, effectiveness of ventricular contraction falls by about 15-20%
Here is a video in which i try and explain atrial fibrillation in an easy to understand way.
What are the symptoms of Atrial fibrillation?
Atrial fibrillation may be completely asymptomatic which means that you may not even know you are in this abnormal rhythm. 25% of people who have AF don’t have any symptoms and in such patients, AF is picked up incidentally by someone feeling the patients pulse and finding it to be irregularly irregular.
Common symptoms are:
- Heart palpitations or a subjective sensation of fluttering or excessive speeding up of the heart.
- Breathlessness – both at rest and especially worse on exertion
- Lightheadedness or dizziness and rarely loss of consciousness
- Tiredness and lethargy
- Very occasionally atrial fibrillation can also cause chest discomfort or tightness and this usually gets worse on exertion
Because AF can sometimes come and go off its own accord, the symptoms are only present when the AF is present. As with the AF, the symptoms are usually of sudden onset and sudden offset.
The symptoms may be due to simply the loss of atrial kick which reduces the pumping effectiveness of the heart by 15-20% but more often because the heart races excessively during the AF.
How is atrial fibrillation diagnosed?
AF can be difficult to diagnose partly because it may be silent/ symptomatic and also because it can come and go.
The first clue is usually the development of symptoms or in asymptomatic patients, the finding of an irregularly irregular pulse. You cannot confidently diagnose AF just by feeling the pulse because sometimes patients may just have occasional extra beats which can make the pulse feel irregular. To make a definitive diagnosis of AF, an electrocardiogram has to be done when the AF is present.
In patients with paroxysmal AF, prolonged ECG monitoring is required to ‘catch’ the AF when it is present.
The most commonly utilised monitor to ‘catch’ AF is a 24 hour holter monitor but for this to be useful you have to have the AF during the 24 hour period that you are wearing the monitor over. Unfortunately 24 hour monitors have a low pickup rate of only about 8%.
There are now available wearable patches which can continuously record the heartbeat for between 14 days (Bardy patch) or 28 days (Zio patch). These have a much higher pickup rate of almost 50%.
Technological advances have now made it possible for smart phone owners to record their own single lead ECGs on their mobile phones. The best known app for this is the Kardia app which is available to buy on Amazon.
For people who have very infrequent episodes of palpitations, the best way to catch the AF is by implanting a monitoring device under the skin. This is called a REVEAL device and is very effective at picking up even very short epodes of AF. A REVEAL device has a battery of unto 2 years and the information it collects can be downloaded by placing a sensor over the skin. Here is the link to a video on the subject of monitors for AF.
What are the different types of atrial fibrillation?
Below are the different types of atrial fibrillation:
Paroxysmal atrial fibrillation
In some patients, especially young patients, AF can come and go off its own accord. These episodes are called ‘paroxysms’ and can last between a few minutes to unto 7 days. These paroxysms may not cause symptoms but when they do, the symptoms tend to be particularly uncomfortable and poorly tolerated by patients. This is partly because the there is a sudden and unpredictable switch from a regular to an irregular rhythm and partly because the patient becomes very fearful because they don’t know when the paroxysm will end.
Many people will notice or identify certain triggers which make them more likely to develop a paroxysm of AF. Common triggers that have been described include:
- Psychological stress
- Physical effort
- Tiredness
- Alcohol (esp red wine and liquor)
- Coffee
- Infections
- Large meals
- Onions
- Nuts
- Chocolate
- Ice cream
- Spiced food
Avoidance of triggers can help reduce paroxysms of AF
Here is a video in which i discuss this in more detail.
Persistent atrial fibrillation
If an AF episode lasts longer than a week, it is described as ‘persistent’. Usually this means that the heart rhythm is unlikely to go back to normal spontaneously and therefore medications or electrical cardioversion treatment is required to get the heart back into a normal rhythm.
Many patients with paroxysmal AF will progress to persistent AF. Patients with significant comorbidities such as diabetes, hypertension and heart failure are a lot more likely to progress to persistent AF.
Permanent atrial fibrillation
Permanent AF is defined as AF that is persistent but attempts to restore normal rhythm have either been unsuccessful or deemed unlikely to succeed.
Many patients with paroxysmal AFib fear the possibility of their AF becoming persistent because of discomfort of symptoms during their paroxysms. Interestingly however, patients actually tend to feel a little better when they go into persistent and then permanent AF because this becomes their normal rhythm and therefore they are no longer subject to sudden unpredictable changes from one rhythm to the another.

